Understanding Periodontal Disease: Protecting Your Gum Health
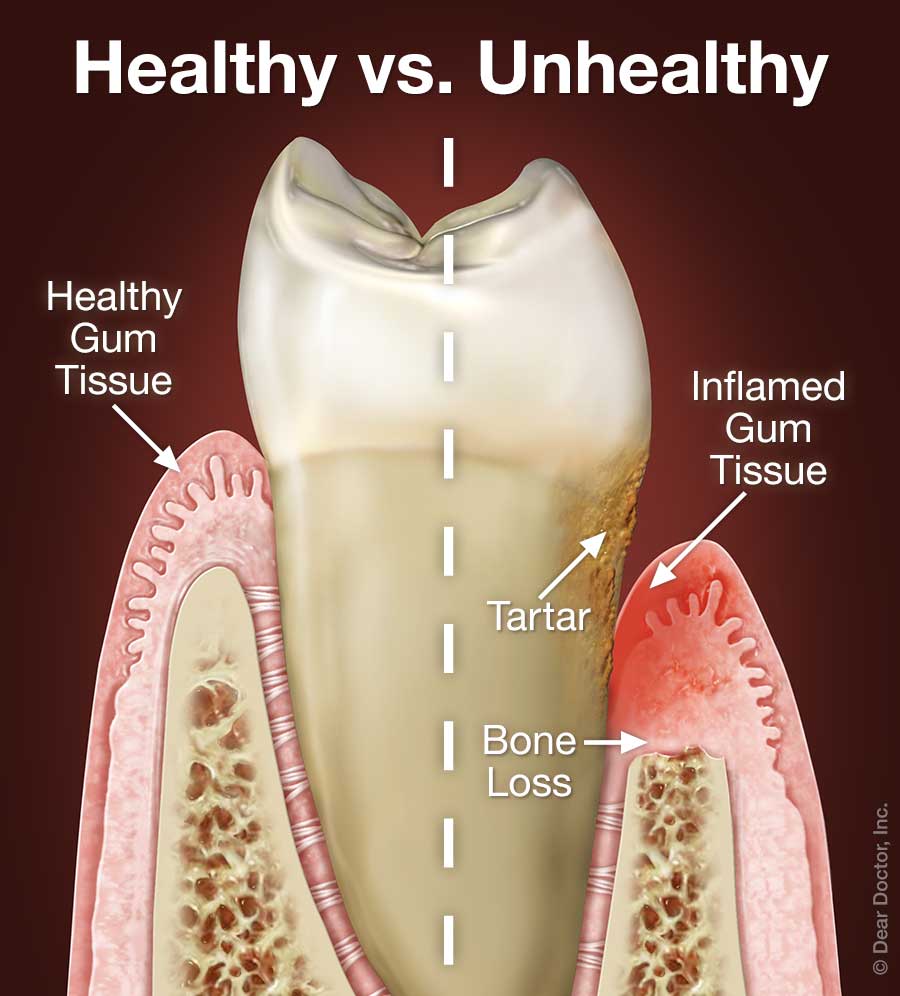
Periodontal disease might sound complex, but it's important to grasp its impact on your oral health. This condition targets the gums and the bone supporting your teeth. Plaque, a mix of food particles, bacteria, and saliva, sticks to your teeth. If not removed, it turns into hard calculus (tartar), which then begins to damage your gums and bone. Signs of periodontal disease include gums that are swollen, red, and bleed easily.
You might be surprised to learn that four out of five people have periodontal disease without even realizing it. Early on, this disease often doesn't cause pain.
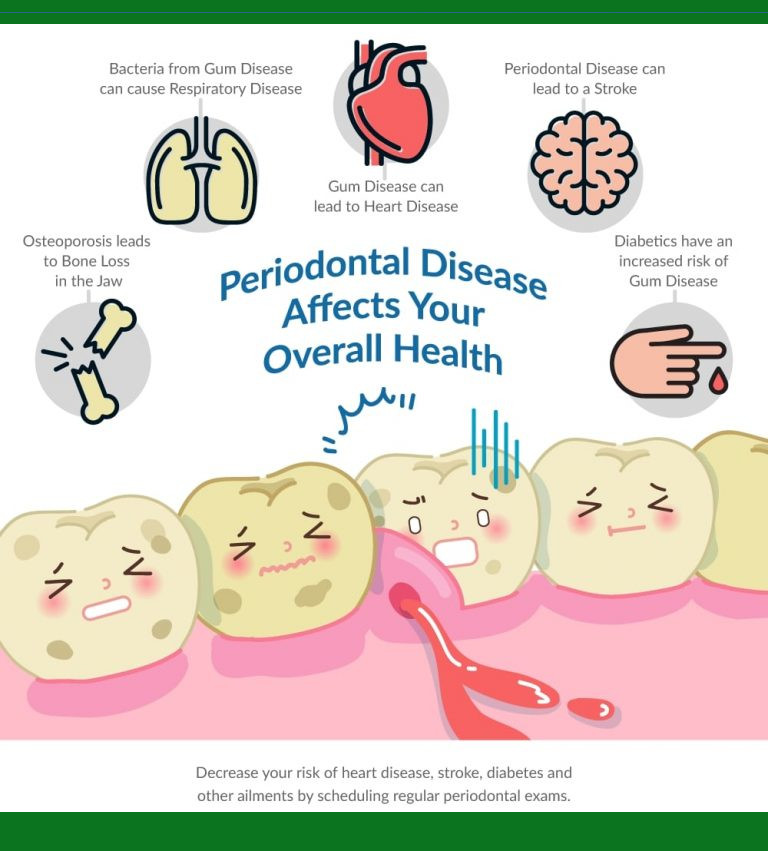
Beyond being the leading cause of tooth loss, researchers suggest a connection between periodontal disease and other health issues like stroke, bacterial pneumonia, diabetes, cardiovascular disease, and pregnancy-related risks. Scientists are investigating if the inflammation and bacteria linked to periodontal disease affect these systemic conditions. Smoking also raises the risk of developing periodontal disease.
However, there's good news. You can reduce your risk of periodontal disease by practicing good oral hygiene, maintaining a balanced diet, and scheduling regular dental visits.
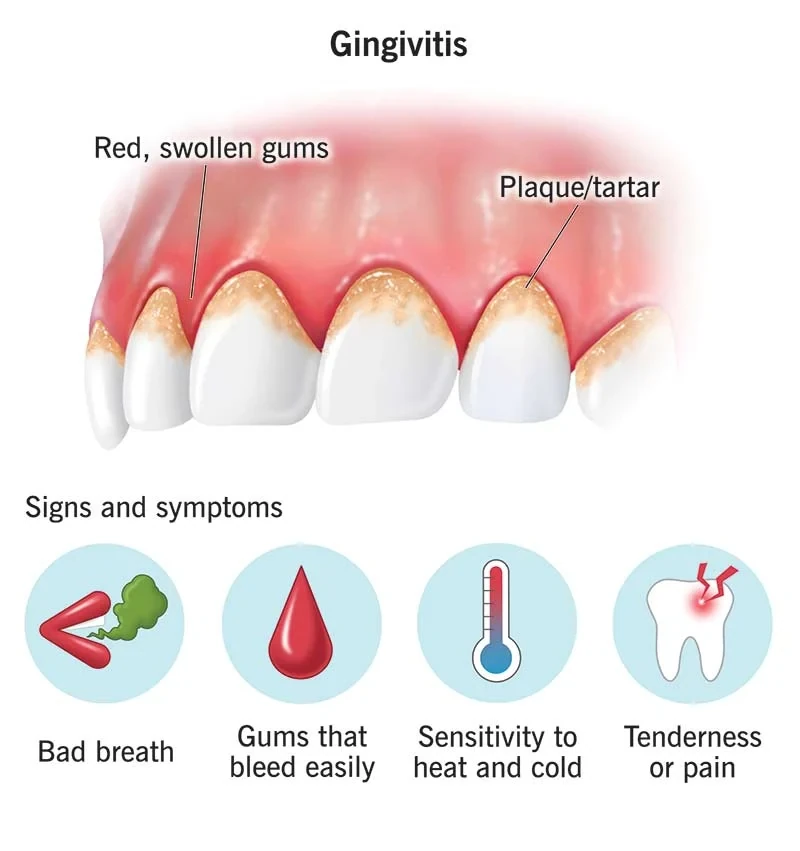
Look out for these signs and symptoms:
- Bleeding Gums: Gums should never bleed, even when you brush vigorously or use dental floss.
- Loose Teeth: Bone loss or weakened periodontal fibers can lead to teeth becoming loose.
- New Gaps Between Teeth: Bone loss can cause gaps to form between your teeth.
- Persistent Bad Breath: Bacteria in the mouth often result in ongoing bad breath.
- Pus Around Teeth and Gums: Presence of pus indicates an infection.
- Receding Gums: Loss of gum around a tooth.
- Red and Swollen Gums: Healthy gums shouldn't be red or swollen.
- Tenderness or Discomfort: Irritated gums and teeth can cause discomfort.
By staying vigilant and maintaining proper oral care habits, you can protect your gums and overall oral health. If you notice any of these signs, don't hesitate to consult a dental professional for guidance. Your oral health is worth it!
 Causes
Causes
Understanding the Causes of Gum Disease: Protecting Your Oral Health

Gum disease, also known as periodontal disease or periodontitis, can lead to tooth loss if not addressed. It begins with inflammation of the gums surrounding the teeth due to toxins in plaque, which triggers a bacterial infection.
The infection settles in the gum tissue, forming pockets between the teeth and gums. Swift treatment by a periodontist can reverse mild inflammation (gingivitis). However, if left untreated, the disease progresses, damaging gums and the jawbone, causing tooth loss. This infection's bacteria can even spread through the bloodstream, affecting other areas of the body.
What Triggers Gum Disease?
Various factors, including genetics and the environment, contribute to gum disease. Preventive measures can significantly reduce the risk of periodontitis. Here are common causes:
- Poor Dental Hygiene: Effective oral hygiene and a balanced diet are key to prevention. Regular dental visits for exams, cleanings, and x-rays are essential. Neglecting oral care allows bacterial toxins to harm gums and bone, leading to gingivitis and periodontitis.
- Tobacco Use: Smoking and tobacco worsen gum disease. Smokers face slower healing and increased calculus (tartar) buildup, deep pockets in gum tissue, and bone loss.
- Genetics: About 30% of people, despite good oral care, have a genetic predisposition to gum disease. Genetic tests can detect susceptibility, prompting early intervention.
- Pregnancy and Menopause: Hormonal changes during pregnancy make gums more sensitive and prone to gum disease. Rigorous oral care is crucial.
- Stress and Diet: Stress weakens the immune system, making it harder to fight infection. A poor diet can also hinder the body's defense against gum infections.
- Diabetes and Medical Conditions: Conditions like diabetes, heart disease, and arthritis worsen gum disease. Diabetes affects the body's ability to control and cure gum infections.
- Teeth Grinding: Grinding teeth damages supporting tissue around them. It's often linked to a misaligned bite, accelerating gum disease.
- Medication: Drugs like contraceptives, heart medicines, and steroids impact teeth and gums, increasing susceptibility to gum disease.
Treating Gum Disease
Periodontists specialize in gum disease treatment and dental implant placement. They perform deep cleaning procedures, prescribe antibiotics, and use tissue grafts for tooth loss. They can also recontour gum tissue for a balanced smile.
Preventing gum disease is crucial for maintaining your natural teeth. Address the causes of gum disease with your dentist to prevent its onset, progression, and recurrence.
For more information about gum disease causes and treatments, don't hesitate to ask your dentist. Your oral health is worth the investment!
 Diagnosing
Diagnosing
Diagnosing Periodontal Disease
Your dentist or dental hygienist will diagnose periodontal disease through a periodontal examination, an important part of your regular dental check-up.
During this examination, a periodontal probe – a small dental tool – is used to measure the sulcus, the space between your tooth and gums. A healthy sulcus is three millimeters or less and doesn't bleed. The probe helps determine if the pockets are deeper than three millimeters. As the disease progresses, these pockets usually become deeper.
Your dentist or hygienist will consider pocket depths, bleeding, inflammation, tooth mobility, and more to make a diagnosis falling into one of these categories:
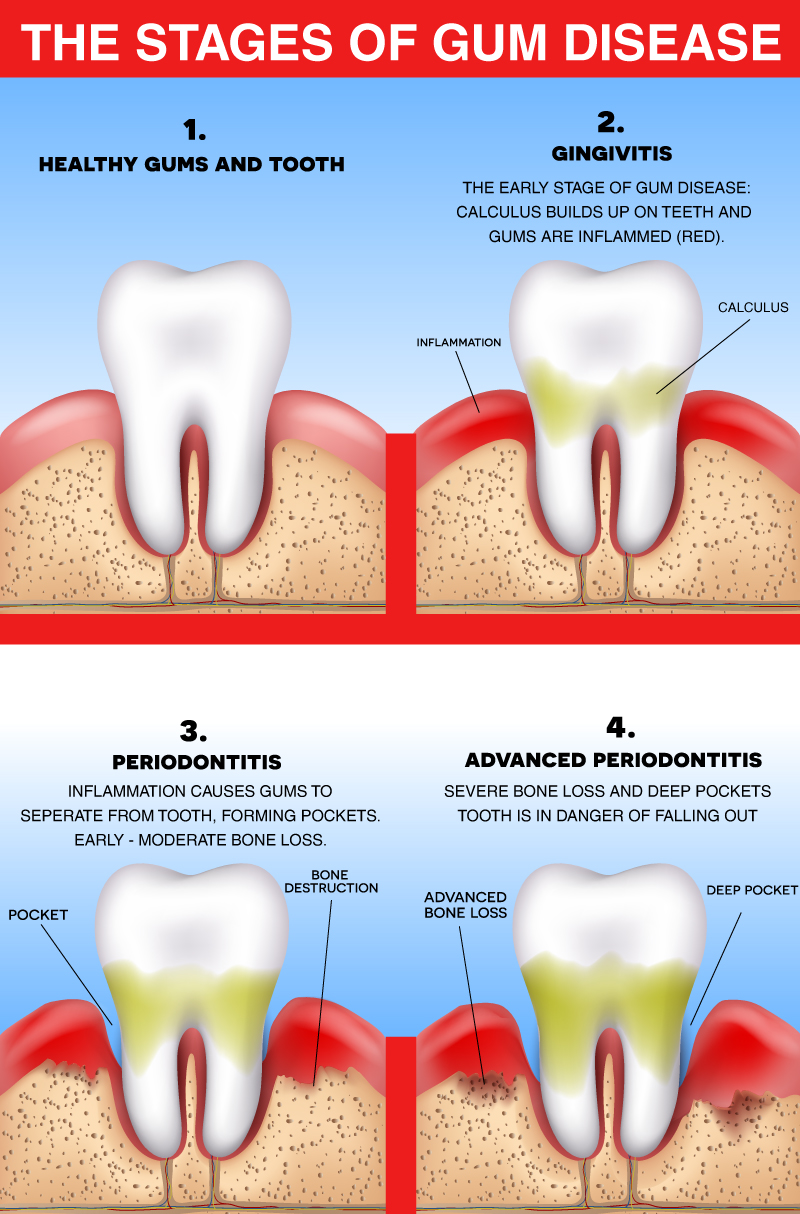
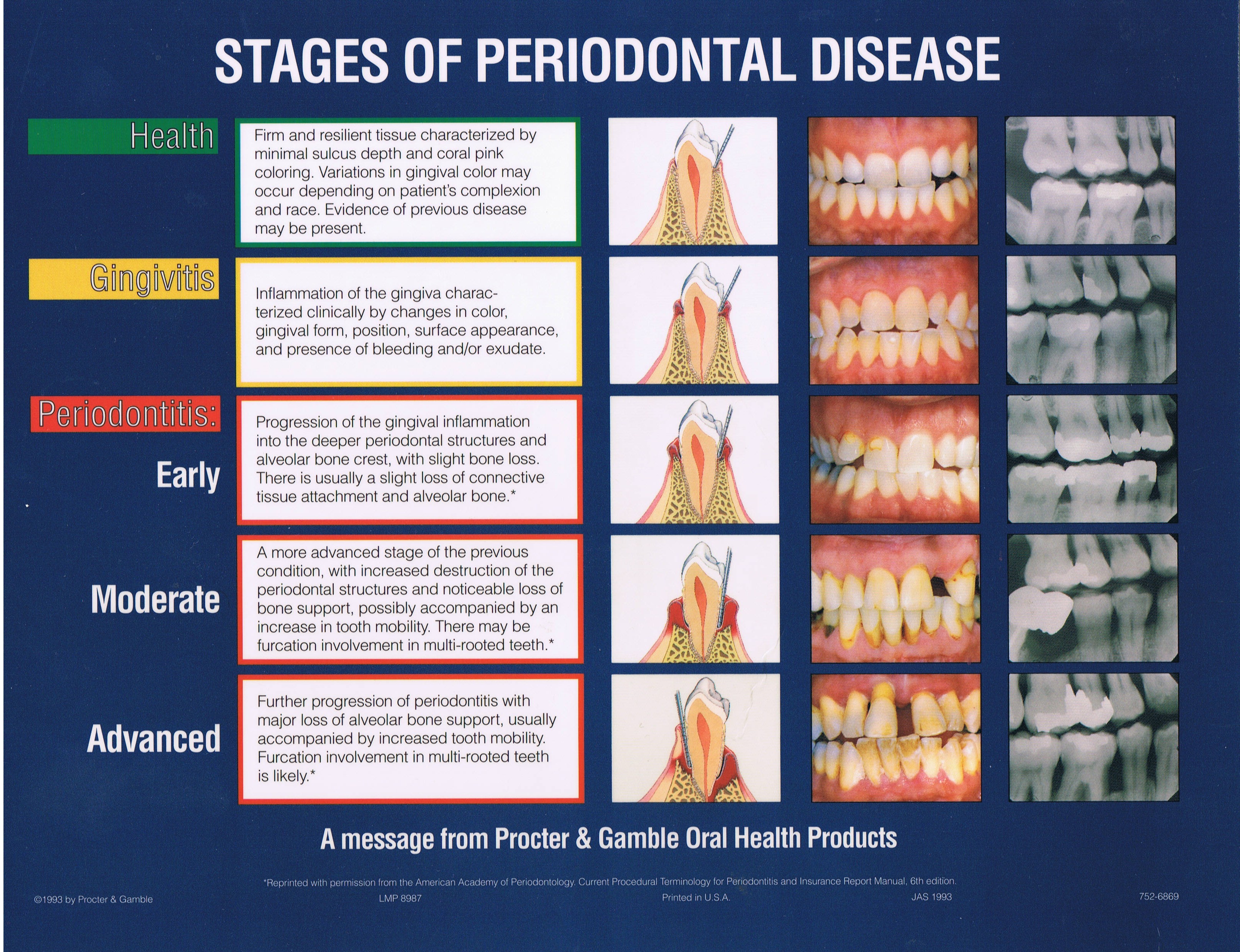
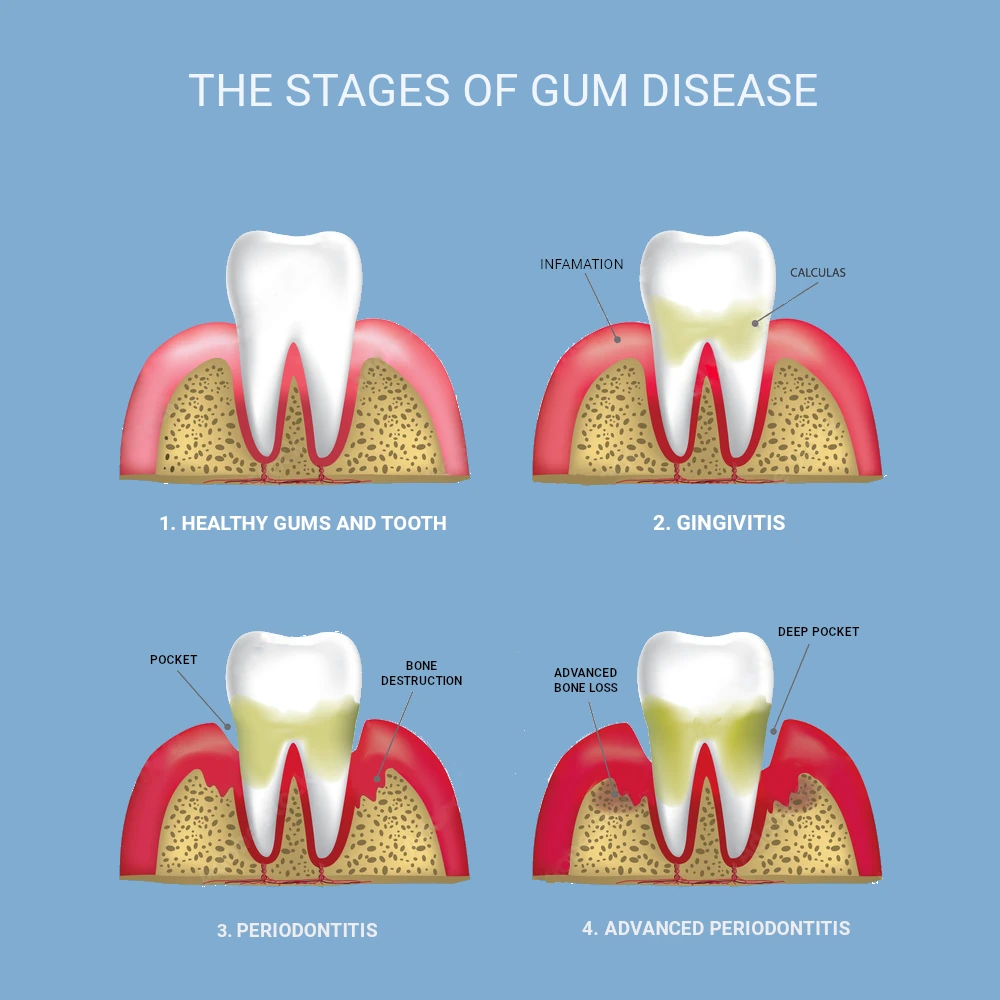
Gingivitis
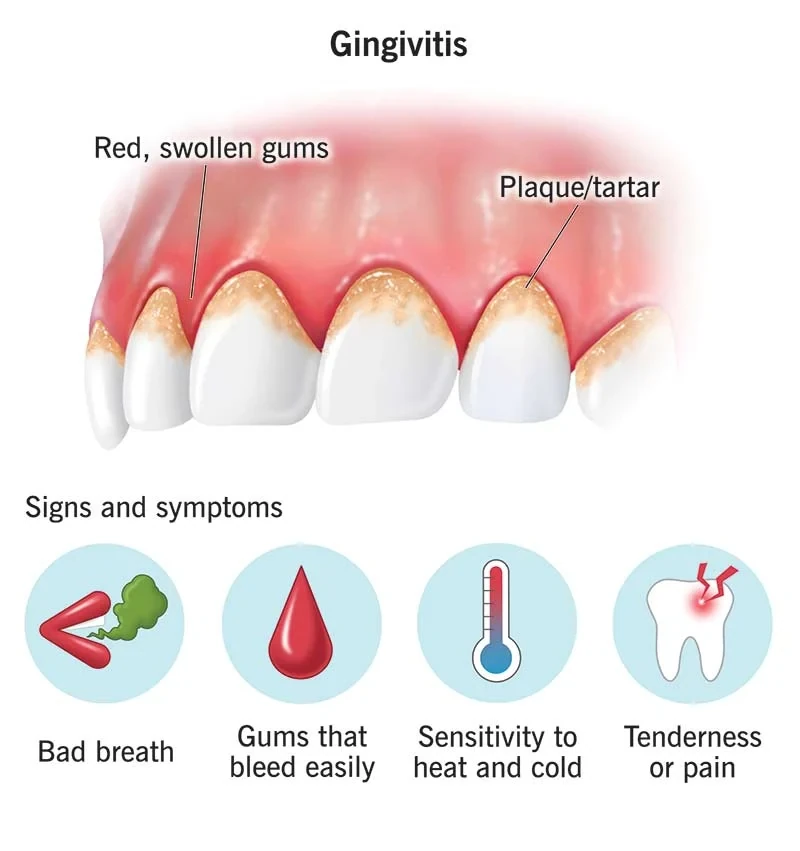
Gingivitis is the initial stage of periodontal disease. Plaque and its toxins irritate the gums, causing tenderness, inflammation, and bleeding.
Periodontitis
Plaque transforms into calculus or tartar. This buildup causes the gums to pull away from teeth, forming deeper pockets filled with bacteria and pus. Gums become inflamed, irritated, and bleed easily. Some bone loss might occur.
Advanced Periodontitis
As gums, bone, and the periodontal ligament continue to deteriorate, teeth lose more support. Without treatment, affected teeth become loose and might be lost. This stage involves generalized moderate to severe bone loss.
 Signs & Symptoms
Signs & Symptoms
Recognizing and Addressing Signs of Gum Disease
Gum disease, also known as periodontal disease, is a serious issue that can lead to tooth loss. It begins when plaque toxins irritate the gums, causing inflammation and infection. This can destroy gum tissue and even affect the bone supporting your teeth. Regular dental checkups are crucial to catch and treat gum disease early.
Common Signs & Symptoms
Gum disease can progress without pain, making regular checkups important. Watch out for these signs:
- Bleeding Gums: Bleeding while brushing, flossing, or eating is a common sign of infection due to plaque toxins.
- Pain, Redness, or Swelling: Swollen, red, or painful gums without an apparent cause might indicate an infection that needs treatment.
- Longer-Looking Teeth: Gum disease can cause gum recession, making teeth appear longer and changing your smile.
- Bad Breath: Debris and bacteria in deep gum pockets can cause bad breath.
- Loose Teeth: As bone is destroyed, teeth can become loose or shift.
- PusPus between teeth indicates an ongoing infection.
Treating Gum Disease
Halting gum disease early is crucial. Dentists assess your mouth's condition and treat the infection using antibiotics and nonsurgical or surgical procedures. Moderate cases may involve scaling and root planing to clean pockets under the gums. Severe cases may require laser treatment, tissue & bone grafting, or pocket elimination surgery.
To learn more about gum disease signs and treatments, feel free to contact us. Your oral health matters!
 Periodontal and Diabetes
Periodontal and Diabetes
Understanding the Connection Between Diabetes and Gum Disease
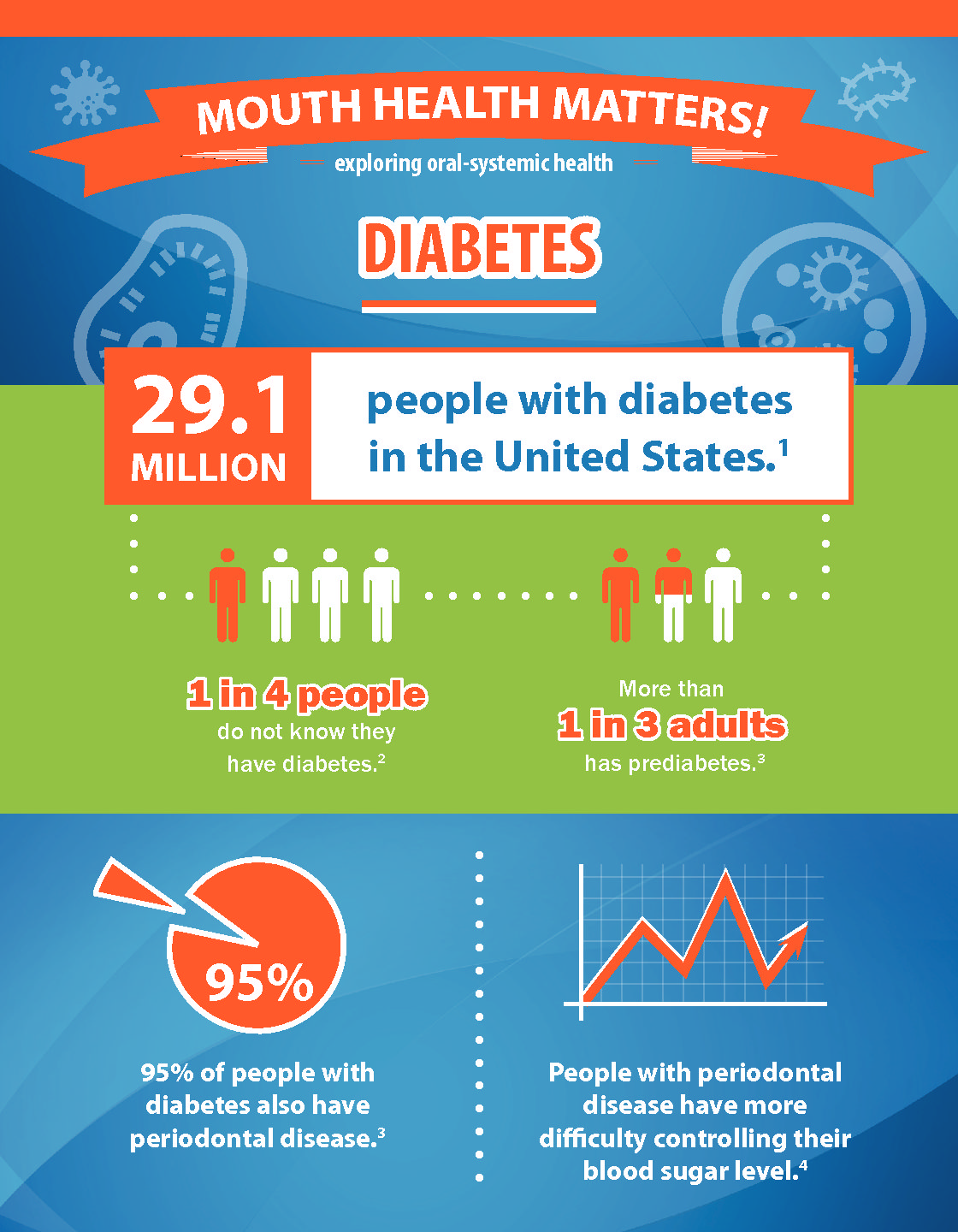
Did you know that diabetes can make you more prone to infections? People with diabetes are at a higher risk of developing periodontal disease, also known as gum disease. This is often considered the sixth complication of diabetes, especially when diabetes isn't well managed.
Periodontal disease is a serious condition that can lead to tooth loss if not treated. It starts with a bacterial infection in the gums surrounding your teeth. The bacteria cause the gums to recede, and the infection can even reach the underlying bone.
Diabetes leads to high levels of sugar in the blood. If not properly controlled, it can harm your heart and cause stroke. The connection between diabetes and gum disease can worsen both conditions if not managed.
Here's how diabetes and gum disease are linked:
- Increased Blood Sugar: Periodontal disease can raise sugar levels in the body, making it hard for diabetics to control their blood sugar. High sugar levels in the mouth feed bacteria that worsen gum infections.
- Blood Vessel Thickening: Diabetes thickens blood vessels, hindering the delivery of nutrients and removal of waste. This weakens gum tissue, leading to infections.
- Smoking: Smoking harms oral health and increases gum disease risk. Diabetic smokers have an even higher risk.
- Poor Oral Hygiene: Diabetics must maintain excellent oral health. Neglecting brushing and flossing can worsen gum infections.
Diagnosis and Treatment
If you have diabetes, see your dentist twice a year. Simple treatments can lower your HbA1c count by up to 20% in six months.
Your dentist will assess your dental and family history, take X-rays, and work with other doctors if needed. Non-surgical treatments include scaling to remove tartar and root planing to smooth tooth roots. Antibiotics may be used to promote healing.
Proper home care and oral maintenance are crucial. If you have questions about diabetes and gum disease, contact our office. We're here to help you maintain your oral and overall health.
 Periodontal, Heart Disease and Stroke
Periodontal, Heart Disease and Stroke
Connecting Periodontal Disease, Heart Disease, and Stroke
It might surprise you, but there's a connection between periodontal disease, heart disease, and stroke. Research has found that people with gum disease are nearly twice as likely to also have coronary heart disease. And oral infections increase the risk of stroke. Those diagnosed with acute cerebrovascular ischemia often have some level of gum disease.
Periodontal disease is a condition where bacteria infect the gums around the teeth. These bacteria start above and below the gumline, causing the tissue to pull away from the teeth. If left untreated, it can form deep pockets between the gums and teeth, damaging the underlying jawbone and causing teeth to shift or even detach.
Coronary heart disease happens when fatty proteins build up in the coronary arteries, making them thicker. This limits oxygen to the heart and forces it to work harder. Clots can form, blocking blood flow and nutrients, leading to heart attacks.
Why Are They Linked?
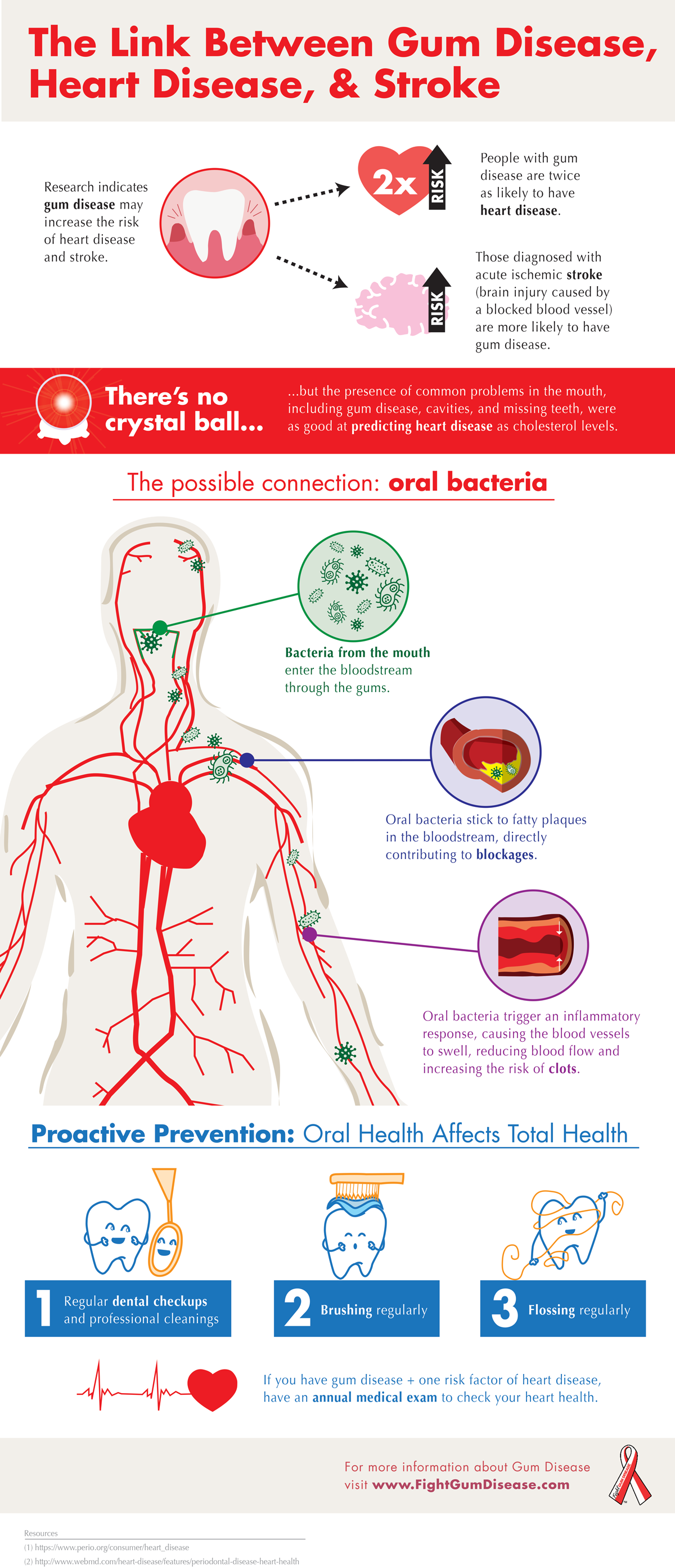
Periodontal disease can worsen existing heart issues. Periodontists and cardiologists often work together to treat both conditions. Here are some theories about the link between heart disease, stroke, and gum disease:
- Oral Bacteria and the Heart: Certain periodontal bacteria enter the bloodstream and stick to fatty plaques in heart blood vessels. This can lead to clot formation and danger.
- Inflammation: Gum disease causes inflammation in gum tissue, increasing white blood cell count and C-reactive protein levels. Higher levels of this protein are linked to heart disease.
- Infection Susceptibility: Those with high oral bacteria levels might have weaker immune systems and inflammatory responses, contributing to heart disease onset.
Diagnosis and Treatment
Since gum disease can increase heart attack and stroke risk, it's vital to seek treatment. A periodontist will examine your teeth, gums, and jawbone. X-rays help assess bone loss.
Deep cleaning treatments, like scaling and root planing, remove tartar from gum pockets. Antibiotics may be prescribed to destroy bacteria and prevent infection spread. Regular cleanings and good home care can prevent gum disease.
If you're concerned about the link between gum disease and heart issues, reach out to our office. We're here to help you understand and manage your oral and overall health.
 Periodontal and Osteoporosis
Periodontal and Osteoporosis
Link Between Periodontal Disease and Osteoporosis
Periodontal disease, characterized by gradual loss of gum and jawbone support, is a leading cause of tooth loss among adults. It happens when toxins in plaque irritate the soft tissue around teeth, leading to gum and bone damage. Osteoporosis, a bone disease mostly affecting postmenopausal women, weakens bones and lowers bone mineral density. Studies have found connections between these two conditions.
A 1995 study at the University of New York at Buffalo revealed that postmenopausal women with osteoporosis had an 86% higher likelihood of developing periodontal disease.
Reasons for the Connection
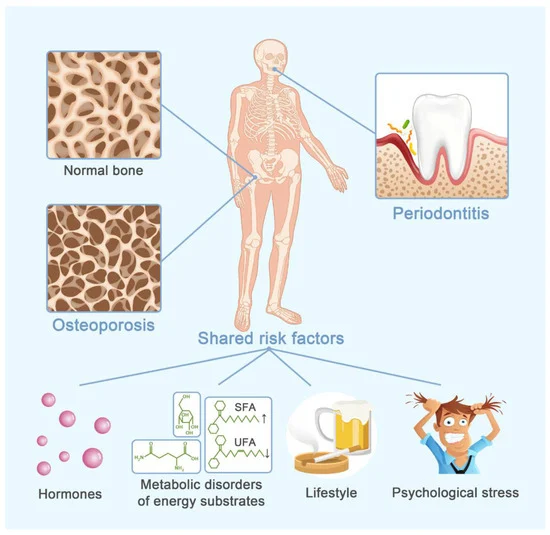
While research is ongoing, here are some connections researchers have identified between osteoporosis and periodontal disease:
- Estrogen Deficiency: Menopause leads to estrogen deficiency, which speeds up bone loss in the mouth. This deficiency accelerates the destruction of teeth-stabilizing fibers and tissues.
- Low Bone Density: Osteoporosis weakens bones, and inflammation from periodontal disease makes already weakened bones more prone to break down. This makes periodontitis more progressive in those with osteoporosis.
Diagnosis and Treatment
Early diagnosis is crucial for managing both osteoporosis and periodontal disease. Once diagnosed, the dentist and doctor can work together to control both conditions effectively.
Here are methods used for diagnosis and treatment:
- Dental X-rays: X-rays screen for bone loss in the upper and lower jaw. Dentists can then intervene to prevent and treat periodontal disease, which in turn helps manage osteoporosis.
- **Estrogen Supplements: Postmenopausal women can receive estrogen supplements to lower attachment loss rate and reduce gum inflammation, protecting teeth from periodontal disease.
- Risk Factor Assessment: Dentists and doctors monitor those at higher risk for both conditions using family history, medical history, X-ray results, current medications, and modifiable risk factors. Education, support, and prescription medications can help manage factors like tobacco use, obesity, poor diet, and estrogen deficiency.
For any questions about the link between periodontal disease and osteoporosis, feel free to reach out to our practice. We're here to help you understand and manage your oral and overall health.
 Periodontal and Respiratory Disease
Periodontal and Respiratory Disease
Connection Between Periodontal Disease and Respiratory Health
Periodontal disease, also known as periodontitis or gum disease, has been linked to respiratory diseases in recent research. Studies have found that periodontal disease might worsen conditions like chronic obstructive pulmonary disease (COPD) and could even contribute to the development of pneumonia, bronchitis, and emphysema.
Periodontal disease starts as a bacterial infection that targets gum tissue. Bacteria in plaque gather in the gums, leading to inflammation and destruction of both gum and bone tissue. As the disease progresses, gums may recede and teeth might seem longer. If left untreated, bone erosion weakens the foundation for teeth, potentially causing them to become loose or even leading to tooth loss.
Several respiratory diseases are associated with periodontal disease, including pneumonia, COPD, and bronchitis. Inhaling tiny droplets from the mouth into the lungs can trigger bacterial respiratory infections. COPD is a serious condition that can be fatal.
Reasons for the Connection
Although the link between respiratory disease and periodontal disease might sound surprising, evidence supports it. Here are some reasons behind this connection:
- Bacterial Spread*: The specific oral bacteria causing periodontal disease can reach the lower respiratory tract. Once in the lungs, these bacteria can lead to pneumonia and worsen conditions like COPD.
- Low Immunity: People with chronic respiratory problems often have weakened immunity, allowing oral bacteria to thrive above and below the gum line. This not only speeds up periodontal disease but also increases the risk of developing conditions like emphysema, pneumonia, and COPD.
- Modifiable Factors: Smoking is a major cause of COPD and other respiratory conditions. Tobacco use also damages gums, slowing healing, deepening gum pockets, and accelerating attachment loss. While smoking isn't the sole cause of periodontal disease, it's a factor to avoid.
- Inflammation: Periodontal disease causes inflammation in oral tissues. The same bacteria causing irritation might also contribute to lung lining inflammation, limiting airflow to and from the lungs.
Diagnosis and Treatment
When both respiratory disease and periodontal disease are present, a team approach involving both the dentist and doctor is crucial. Various non-surgical and surgical treatments are available based on the specific condition of teeth, gums, and jaw.
The dentist can assess inflammation and tissue loss and treat the bacterial infection. Procedures like scaling remove debris, while root planing smooths tooth roots to eliminate lingering bacteria. Antibiotics might be applied to promote healing and reduce infection risk.
Managing periodontal disease offers two benefits: improved oral health and reduced respiratory infections associated with conditions like COPD.
If you have concerns about respiratory or periodontal disease, don't hesitate to ask your dentist. They can provide valuable information and guidance for maintaining your oral and respiratory health.
 What is Periodontal (Gum) Disease?
What is Periodontal (Gum) Disease?
Understanding Different Types of Gum Disease and Their Treatments
Periodontal disease, also called gum disease or periodontitis, can lead to tooth loss if not treated. It starts with toxins in plaque attacking the gums, causing an infection that affects the supporting bone. If left untreated, gums recede, teeth become unstable, and tooth loss occurs. This disease is the leading cause of tooth loss in adults and should not be ignored.
Gum Disease Types and Treatments
- Gingivitis: Mildest form, caused by plaque toxins. Pregnant women, diabetics, and others are at risk. Treated with home care, professional cleaning, antibiotics, and mouthwashes.
- Chronic Periodontal Disease: Common in those over 45. Inflammation below gums, gradual gum recession. Treated with scaling, root planing, and surgeries if needed.
- Aggressive Periodontal Disease: Fast loss of gum and bone tissue. Smokers and those with family history at risk. Treated similarly to chronic type but may need more surgeries.
- Periodontal Disease Relating to Systemic Conditions: Linked to diseases like heart disease, diabetes, and respiratory problems. Control underlying condition, then treat gum disease.
- Necrotizing Periodontal Disease: Rapidly worsens, more common in HIV, immunosuppression, or smoking. Consult with a physician, use antibiotics, medicated mouthwash, and other medicines.
Preventing gum disease is key to keeping your teeth. If you have questions about types of gum disease and their treatments, talk to your dentist. Your oral health is vital!
 Treatment
Treatment
Treating Periodontal Disease
The treatment you receive for periodontal disease depends on its type and severity. Your dentist and dental hygienist will assess the condition and suggest the right treatment.
As periodontal disease advances, the space between your tooth and gums, known as the sulcus or pocket, gets filled with bacteria, plaque, and tartar. These irritants can harm the nearby tissues and even the bone that supports your teeth.
If the disease is caught early in the gingivitis stage and hasn't caused damage yet, one to two regular cleanings will be recommended. You'll also receive guidance on improving your daily oral hygiene practices and keeping up with dental cleanings.
For more advanced stages, a deep cleaning called scaling and root planing will be suggested. This process is done one section of the mouth at a time while numbed. During scaling, tartar, plaque, and toxins are removed from above and below the gum line. Root surfaces are smoothed during planing. This helps the gum tissue heal and reduces pocket size. Medications, specialized mouth rinses, and an electric toothbrush might be advised to manage infection and aid healing.
If pockets don't heal after scaling and root planing, you might need periodontal surgery to lessen pocket depth for better cleaning. Your dentist might also refer you to a periodontist, a specialist in gum and bone support.
 Maintenance
Maintenance
Maintaining Your Oral Health
Did you know that it takes just twenty-four hours for plaque on your teeth to become calculus (tartar) if not removed? Daily cleaning at home helps manage plaque and tartar, but certain areas are harder to clean and need special care.
Once your periodontal treatment is finished, your dentist and dental hygienist will advise regular maintenance cleanings (periodontal cleanings), typically about four times a year. During these cleanings, they'll check the health of your pocket depths meticulously. Plaque and calculus that's tough to remove daily will be taken out from above and below your gum line.
In addition to the cleaning and checkup, your appointment will usually include:
- Examination of x-rays: These are vital for spotting decay, tumors, cysts, and bone loss. X-rays also help assess tooth and root positions.
- Inspection of existing restorations: Current fillings, crowns, etc., are examined.
- Detection of tooth decay: All tooth surfaces are checked for decay.
- Oral cancer screening: The face, neck, lips, tongue, throat, cheek tissues, and gums are examined for any signs of oral cancer.
- Oral hygiene suggestions: Recommendations are given for oral hygiene aids as needed, like electric toothbrushes, special brushes, fluorides, rinses, etc.
- Teeth polishing: Stains and plaque that brushing and scaling miss are removed.
Maintaining good oral hygiene and having regular periodontal cleanings are crucial for dental health and to keep periodontal disease in check!
